Poster Details
Poster Submitter: Bridget McGrath, MPAS, PA-C, FHM
Department: Hospital Medicine
Email Address: bmcgrath@bsd.uchicago.edu
Role: Staff (non-nurse)
Project Lead: Dana Caruso, MMA, PA-C / Obstetrics and Gynecology
Project Collaborators:
- Frank Umbriaco, MSN, BS AGACNP – BC / Staff (non-nurse)
- Charina Alcain, ACNP-BC, DNP / Staff (non-nurse)
- Meghan Day, MPAS, PA-C / Staff (non-nurse)
- Dorothy Pietrowski, MSN, ACNP, ONP-C / Staff (non-nurse)
- Greg Tomczyk, PA-C / Staff (non-nurse)
- Michele Rubin, MSN, CNS-BC, CGRN / Staff (non-nurse)
- Reasheal Watts, MSN, AGACNP-BC / Staff (non-nurse)
- Bridget McGrath, MPAS, PA-C / Staff (non-nurse)
- Alisa Heitman, MSN, NP-C / Staff (non-nurse)
Departments Included in Project: Ambulatory Services, Anesthesia, Family Medicine, Gynecology, Inpatient Services, Medicine, Neurology, Obstetrics, Orthopedics, Surgery,
Project Classification: Effectiveness
Project Notes/Comments:
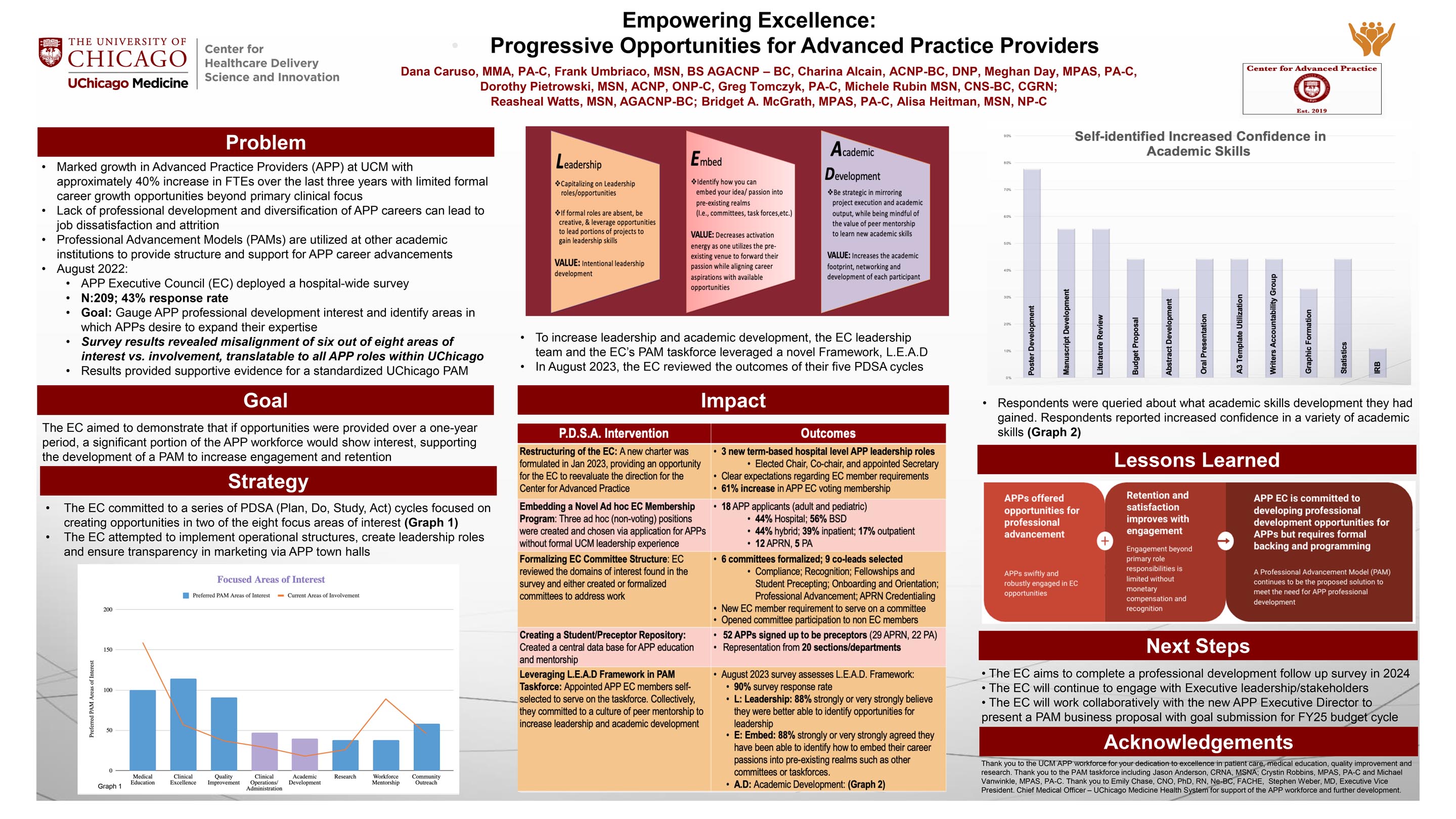
This project focused on creating professional development opportunities for Advanced Practice Providers (APPs). APPs have enjoyed a marked growth as a profession and are continually noted as vital members of the health care system. APPs include physician assistants (PA) and advanced practice registered nurses (APRN), which is an umbrella term for nurse practitioners (NP), certified registered nurse anesthetists (CRNA), certified midwives (CNM), and clinical nurse specialists (CNS). Despite clinical acceptance, a recent study in the Journal of Hospital Medicine found that APPs are less frequently involved (<50%) in teaching, research, quality improvement (QI) and leadership training suggesting underutilization of the APP workforce in these realms.
Does the work incorporate equity?
According to to 2021 NCCPA statistical data 25% of surveyed PAs reported their work as not professionally challenging or satisfying and 40.2% identified feelings of professional burnout as factors influencing their decision to leave their principal clinical work setting.2 Similarly, a 2021 survey of APRNs, inclusive of NPs, CRNAs, and CNMs, found 33% of APRNs had experienced burnout at some point in their careers, and 26% of APRNs currently endorsed burnout.3 APP burnout not only impacts personal and professional wellbeing, but studies demonstrate a direct impact on work engagement. A study in 2020 further explored burnout and job stressors among advanced practice providers and found statistically significant correlations between burnout and work engagement. These findings help understand the strategic nature of balancing organizational priorities and while improving engagement through programs that encourage professional growth. As we built out these programs were ensured equity in marketing and were inclusive of all 5 APP Disciplines. Our hope is through better engagement and decreased burnout this positively impacts patient care.
Does this work address any of the UChicago Medicine quality priorities as listed on the Clinical Excellence Scorecard?
Patient Experience

Leave A Comment